Sacroiliac Joint Dysfunction
Sacroiliac Joint Dysfunction

Introduction
A painful sacroiliac joint is one of the most common causes of mechanical low back pain. Sacroiliac (SI) joint dysfunction is a term that is used to describe the condition – because it is still unclear why this joint becomes painful and leads to low back pain. Sacroiliac joint dysfunction can be a nuisance, but it is seldom dangerous and rarely leads to the need for surgery. Most people who suffer from this problem can reduce the pain and manage the problem with simple methods.
Anatomy
At the lower end of the spine, just below the lumbar spine lies the sacrum. The sacrum is a triangular shaped bone that is actually formed by the fusion of several vertebrae during development. The sacroiliac (SI) joint sits between the sacrum and the iliac bone (thus the name “sacroiliac” joint). You can see these joints from the outside as two small dimples on each side of the lower back at the belt line.

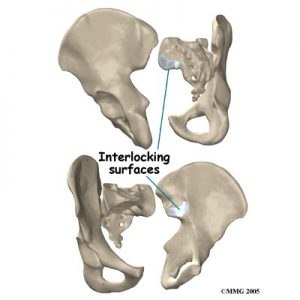
The SI joint is one of the larger joints in the body. The surface of the joint is wavy and fits together similar to the way Legos® fit together. Very little motion occurs in the SI joint. The motion that does occur is a combination of sliding, tilting and rotation. The most the joint moves in sliding is probably only a couple of millimeters, and may tilt and rotate two or three degrees.
The SI joint is held together by several large, very strong ligaments. The strongest ligaments are in the back of the joint outside of the pelvis. Because the pelvis is a ring, these ligaments work somewhat like the hoops that hold a barrel together. If these ligaments are torn, the pelvis can become unstable. This sometimes happens when a fracture of the pelvis occurs and the ligaments are damaged. Generally, these ligaments are so strong that they are not completely torn with the usual injury to the SI joint.

The SI joint hardly moves in adults. During the end of pregnancy as delivery nears, the hormones that are produced causes the joint to relax. This allows the pelvis to be more flexible so that birth can occur more easily. Multiple pregnancies seem to increase the amount of arthritis that forms in the joint later in life. Other than the role the joint plays in pregnancy, it does not appear that motion is important to the function of the joint. The older one gets, the more likely that the joint is completely ankylosed, a term that means the joint has become completely stiffened with no movement at all. It appears that the primary function of the joint is to be a shock absorber and to provide just enough motion and flexibility to lessen the stress on the pelvis and spine.
Causes
There are many different causes of SI joint pain. Pregnancy may be a factor in the the development of SI joint problems later in life. Also, if a person has one leg shorter that the other, the abnormal alignment may end up causing SI joint pain and problems. Often, an exact cause leading to a painful SI joint condition can’t be found.

Injury to the SI joint is thought to be a common cause of pain. Injury can occur during an automobile accident. One common pattern of injury occurs when the driver of a vehicle places one foot on the brake before a collision. The impact through the foot on the brake is transmitted to the pelvis causing a twisting motion to this side of the pelvis. This can injure the SI joint on that side resulting in pain. A similar mechanism occurs with a fall on one buttock. The force again causes a twisting motion to the pelvis and may injure the ligaments around the joint.
Symptoms

The most common symptoms from SI joint dysfunction are low back and buttock pain. The pain may affect one side or both SI joints. The pain can radiate down the leg all the way to the foot and may be confused with a herniated disc in the lumbar spine. The pain may radiate into the groin area. People often feel muscle spasm in one or both of their buttocks muscles.

Problems with the SI joint may make sitting difficult. Pain in one SI joint may cause a person to sit with that buttock tilted up. It is usually uncomfortable to sit flat in a chair.

Diagnosis
Diagnosis begins with a complete history and physical exam. Your Osteopath will ask questions about your symptoms and how the pain is affecting your daily activities. Your Osteopath will also want to know what positions or activities make your symptoms worse or better. You will be asked questions about any injuries in the past and about any other medical problems you might have such as any arthritis that runs in the family.

An Osteopath then will examine you by checking your posture, how you walk and where your pain is located. These will help to see which back movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are also to be tested because it is difficult to distinguish pain coming from the SI joint from pain coming from other spine conditions.

X-rays might be ordered for both the low back and pelvis. X-rays can give your Osteopath an idea about how much wear and tear has occurred in the SI joint. X-rays of the lumbar spine and hips are also helpful to rule out problems in these areas that may act and look like SI joint dysfunction.
Other radiological tests may be useful as well. The magnetic resonance imaging (MRI) scan can be used to look at the lumbar spine and pelvis in much more detail and to rule out other conditions in the area. The MRI scan uses magnetic waves rather than x-rays and shows a very detailed picture of the soft tissues of the body.
General advice
DO• Listen to your body. Try to remain as active as possible within your comfort limits but avoid activities that make the pain worse. • Rest more frequently. • Ask for and accept help from others, involving partner, family and friends as possible. • Sleep on your side with a pillow between the legs. Turn over with your knees together and squeezing your buttocks. Keep knees and shoulders in line to avoid twisting. • Sit down to do things that you would normally stand for e.g. getting dressed and undressed; ironing… • Go upstairs one step at a time with the less painful leg first. Go downstairs leading with the most painful leg. • Wear flat, supportive shoes.
AVOID • Standing on one leg to put on trousers or tights. • Stooping or bending during activities • Movements that involve separation of your legs e.g. getting in/out of bed; getting in/out of car; if swimming avoid breast stroke; take small steps when walking; consider alternative positions for intercourse. • Asymmetrical positions of the pelvis e.g. avoid twisting movements and sitting cross-legged. • Sitting on the floor or low chairs or soft, deep couches. • Avoid lifting heavy weights. • Using your feet to move objects on the floor.
Nonsurgical Treatment
Doctors often begin by prescribing nonsurgical treatment for SI joint dysfunction. In some cases, doctors simply monitor the patient’s condition to see if symptoms improve. Anti-inflammatory medications, such as ibuprofen and naproxen, are commonly used to treat the pain and inflammation in the joint. Acetominiphen (for example, Tylenol) can be used to treat the pain, but it will not control the inflammation.
Patients often work with a physical therapist or osteopath. After evaluating your condition, a therapist can assign positions and exercises to ease your symptoms. The therapist may design an exercise program to improve the strength and control of your back and abdominal muscles. Osteopaths are trained in manipulative techniques that attempt to treat the pain in this manner. You may be able to learn how to adjust your SI joint yourself and ease the symptoms.

Most commonly used osteopathic technique for pelvic manipulation is Anterio – Posterior Lumbopelvic Manipulation AKA Chicago
https://www.physio-pedia.com/Lumbopelvic_Manipulation_technique
Your doctor may ask that you rest your back by limiting your activities. The purpose of this is to help decrease inflammation and calm the muscle spasm. Some patients benefit from wearing a special brace called a sacroiliac belt. This belt wraps around the hips to hold the sacroiliac joint tightly together, which may ease your pain.

If conservative treatment is unsuccessful, injections may be suggested by your doctor. As described above, injections are used primarily to confirm that the pain is coming from the SI joint. A series of cortisone injections may be recommended to try to reduce the inflammation in and around the SI joint. Cortisone is a powerful anti-inflammatory medication that is commonly used to control pain from arthritis and inflammation. 
Another procedure that has been somewhat successful is called radiofrequency ablation. After a diagnostic injection has confirmed that the pain is coming from the SI joint, the small nerves that provide sensation to the joint can be “burned” with a special needle called a radiofrequency probe. In theory, this destroys any sensation coming from the joint, making the joint essentially numb. This procedure is not always successful. It is temporary but can last for up to two years. It can be repeated if needed.
Sourse: www.eorthopod.com

Colgan Osteopathy in Kettering Northamptonshire
Colgan Osteopathy in Hatfield, Hertfordshire
To book an appointment, call 07738493974 or book online