Temporomandibular Disorder (TMD)
Temporomandibular Disorder (TMD) is a broad term that encompasses disorders of the temporomandibular joint and its associated anatomical structures. The disorder may be intra-articular, due to inflammation, internal structural changes (internal derangement) or degeneration, or it may be extra- articular due to imbalance or over-activity of the jaw muscles, commonly the muscles of mastication or the cervical muscles. There is a strong correlation between postural dysfunction of the cervical spine and TMD. There are numerous other conditions that can cause pain in the TMJ region. It is important to make an accurate diagnosis to ensure that the correct treatment is given and that potentially serious problems are not overlooked.
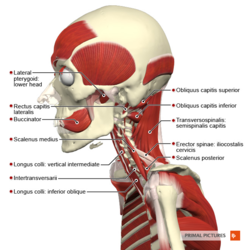
Relevant Anatomy
In an early study on postmortem specimens, it found that the lateral pterygoid muscle was connected to the medial aspect of the joint capsule, meniscus and the condyle pterygoid fovea in more than half of the specimens. It indicated that the muscle might have a specific contribution to the TMD.
Causes of TMD
Intra-Articular Causes
1. Inflammatory conditions within the joint are often caused by direct trauma, such as a blow to the chin or jaw, indirect trauma, such as a whiplash injury, heavy chewing, grinding (bruxism), clenching of the jaw or loss of dental height due to worn down or missing teeth.
- Synovitis – The synovium or the capsule may be inflamed. There is often pain at rest and limited range or pain at the end of range.
- Retrodiscitis – The retrodiscal tissue (the posterior attachment of the articular disc to the mandibular fossa) is highly vascular and innervated and if inflamed, can cause severe pain. The jaw may deviate away from the painful side at rest and with opening.
2. Internal derangement describes conditions where there are structural changes within the joint. This can be caused by direct trauma, such as a blow to the jaw or falling on the chin, indirect tauma, such as a whiplash injury, long term clenching or grinding, heavy or hard chewing or prolonged periods of mouth opening, such as a dental procedure or a general anaesthetic.
- Disc displacement with reduction – The articular disc can become displaced in any direction, but will most commonly displace anteriorly. The disc will be pushed forward during opening and will bunch up. At a certain point in range the disc will reposition or reduce itself causing an audible or palpable click. The jaw will often deviate towards the affected side.
- Disc displacement without reduction – In this more severe version the disc will not reduce causing pain and a loss of range. This is called closed lock. The jaw will often deviate towards the affected side. There will be no click but the patient may report that there was a click at the time when their jaw locked.
3. Arthritis
- Degenerative Arthritis can occur in the TMJ. It can often be seen on plain x-ray or OPG as a flattening of the condylar head, often with some osteophytic formation MRI gives more information with views done in open and closed positions. This shows the position of the joint and disc at the start and end of range. Crepitus can often be felt or can be heard with a stethoscope. It can be age related degeneration, usually seen in the over 50s, or secondary to trauma occurring at a younger age.
- Inflammatory Joint Diseases can affect the TMJ, including rheumatoid arthritis, ankylosing spondylitis, infectious arthritis, Reiter syndrome and gout.
4. Hyper mobility can result in excessive anterior movement of the jaw and the articular disc. This will result in deviation of the jaw away from the affected side. There are usually some clicking sounds in the TMJ and there may or may not be pain. Hyper mobility may be related to connective tissue disorders such as Marfan syndrome or conditions such as Down Syndrome and Cerebral Palsy. Long term hyper mobility can cause the articular disc to elongate and degenerate. The disc can then fail to reduce on closing, causing the TMJ to become stuck in an open position (Open Lock). This can often occur after opening the mouth to an extreme position, such as when singing or yawning or after a prolonged dental procedure.
Extra-Articular Causes
1. Muscle Spasm can cause significant pain and limitation of movement of the jaw. This is referred to as trismus. It often affects one or more muscles, commonly the muscles of mastication, especially masseter, temporalis and the pterygoid muscles. Causes include prolonged dental procedures or anaesthetics where the mouth has been held open for extended periods of time, stress, bruxism and postural dysfunction.
2. Cervical Postural Disorders can cause jaw pain. The anterior belly of the digastric muscle runs from the point of the chin to hyoid bone. This attachment means that when the head is protracted forward digastric will exert a posterior force on the mandible. With prolonged cervical protraction as occurs with poor posture or stress-related posture the mandibular condyle is pushed back against the retrodiscal tissue, eventually causing swelling, pain and gradual degeneration of the disc.
3. Temporal Tendonopathy is caused by excessive contraction of the temporalis muscle usually as a result of bruxism. There is tenderness and swelling of the anterior portion of the temporalis tendon palpable just above the zygomatic arch. There may also be tenderness of the temporalis tendon where it inserts onto the coronoid process, palpable just below the zygomatic arch when the jaw is slightly open.
4. Fractures of the mandible often occur at the mandibular symphysis or the condylar neck. Commonly there will be a fracture of the mandibular symphysis combined with a fracture/dislocation of one or both condyles. The mechanism of injury can be a blow to the jaw or a fall onto the chin. Treatment can usually begin within a week or two of surgery to begin early mobilisation of the TMJ and to restore function.
Diagnosis
There are different clinical protocols used to establish TMD diagnoses but the Research Diagnostic Criteria for TMD (RDC/TMD) could promote the level of consistency between in research studies , it may also be practical in clinical usage.
Assessment of TMD
As with all areas of physiotherapy, a thorough history needs to be taken. The examination should include assessment of the patient’s posture (position of the jaw, tongue and neck); palpation of the TMJ to assess for swelling, muscle spasm and stiffness or hypermobility of one or both TMJ; assessment of range and quality of movement of the jaw and neck, particularly noting any deviation or deflection of the jaw and assessment of the patient’s bite. Also check signs of sleep bruxism (grinding or clenching during sleep). Often the patient will have been told by their sleep partner that they grind their teeth, or their dentist may have noticed excessive wearing of their teeth, or a scalloped edge on the lateral aspects of the tongue. Other signs include waking with teeth clenched, waking with muscle soreness or temporal headache or indentations in the tongue or cheeks If the patient has OPG Xrays or MRI, these can give more information on the condition of the joint and the disc and, if open views are available, on the amount of movement of the joint.
Treatment of TMD
TMD is a recurring, but self limiting condition that tends not to be progressive. Non-invasive, conservative treatments have found to be effective. Physiotherapy treatment is very effective in relieving and managing TMD, even when the symptoms are long-standing and severe. With appropriate physiotherapy most patients will see a significant improvement in their symptoms within 3 to 6 weeks.
Treatment needs to address the issues identified in the assessment. If the patient’s symptoms are acute and inflammatory then their condition is likely to be irritable and one should proceed very gently with the aim of first relieving pain, swelling and muscle spasm. When the pain begins to settle then start to restore jaw movement and alignment. Treatment may include soft tissue releases to affected muscles and joint mobilisation techniques. It is also important to treat any associated neck pain and headaches. Posture correction is essential and should address head, neck, shoulder and tongue position. The patient should be taught exercises to improve coordination, stability and alignment of the jaw.
If the patient has signs of sleep bruxism then should discuss with their dentist whether and occlusal splint would be appropriate for them. Occlusal splints hold the TMJ slightly apart as the patient clenches or grinds, preventing compression of the TMJ. This can help to relax jaw muscles and reduce swelling and inflammation. There is some evidence to supporting the use of splints to reduce long term degeneration of the TMJ, disc and teeth. Other dental problems, such as cavities, that are causing pain or uneven chewing, lack of dental height or missing teeth may also need to be addressed.
The patient should be taught strategies to help them manage their condition. This may include posture education, long-term continuance of their home exercise programme, good sleep habits including sleeping positions, stress management and diet modification – a soft food diet while the condition is acute can help to reduce the pain and swelling more quickly. The patient should also be taught ways to reduce stress on the TMJ by avoiding activities such as resting the chin on the hand, pencil chewing, jaw clenching while awake, wide mouth yawning, nail biting. They should avoid chewy foods, chewing gum, eating foods that need a wide opening like large hamburgers and chewing hard foods such as nuts and apples. Case report suggests early post-operative exercises after temporomandibular joint (TMJ) ankylosis in pediatric patients along with a stringent follow-up to prevent post-operative shrinkage and adhesions.
Manual Therapy
A systematic review was published in 2015 to summarize the effectiveness of manual therapy on signs and symptoms of TMD. It showed that protocols of mixed manual therapy techniques, upper cervical mobilization or manipulation, had considerable evidence for TMD symptom control and improvement in maximum mouth opening. The manual techniques included intra-oral myofascial release and massage therapy on masticatory muscles, atlanto-occipital joint thrust manipulation, and upper cervical spine mobilization.
Therapists should be trained, follow the guidelines and standard procedures to perform the cervical thrust manipulation if it is indicated.
Other Causes of TMJ and Facial Pain
It is important to be aware that there are other causes of pain and dysfunction in the oro-facial region that need to be distinguished from TMD. Below are some of the more common.
1. Referred Pain – Noxious input from the trigeminal nerve, C1, C2 and C3 nerves all feed into the trigeminocervical nucleus in the brainstem and can cause referred pain. “The trigeminocervical nucleus is a region of the upper cervical spinal cord where sensory nerve fibers in the descending tract of the trigeminal nerve (trigeminal nucleus caudalis) are believed to interact with sensory fibers from the upper cervical roots. This functional convergence of upper cervical and trigeminal sensory pathways allows the bidirectional referral of painful sensations between the neck and trigeminal sensory receptive fields of the face and head.” This means that any part of the head and upper neck can refer pain to any other part. Careful examination of the patient’s TMJ and neck is very important to ensure that all structures contributing to the condition are identified and treated.
2. Neuropathic Pain
- Trigeminal Neuralgia (Tic Doloreaux) is characterised by severe, shooting pain in the distribution of one or more of the three branches of the trigeminal nerve (Cranial Nerve V). It can be caused by sensatisation of the trigeminal nerve or by compression or impingement of the nerve. It is usually one sided.
- Trigeminal Neuritis is due to inflammation of the trigeminal nerve.
- Complex Regional Pain Syndrome is characterised by a continuous burning pain, not necessarily in the path of a particular nerve. It is usually secondary to a traumatic injury and is worsened by fear or anxiety. As it worsens there can be skin changes and sweating in the area of pain. These patients need early referral to a pain specialist to prevent worsening of their condition.
- Bell’s Palsy is a palsy of the facial nerve (Cranial Nerve VII). In approximately 70% of cases it resolves withing 6 to 8 weeks. Early treatment with prednisone can significantly reduce the recovery time. Physiotherapy may be required if there is residual weakness.
- Shingles (Herpes Zoster) usually affects the opthalmic division of the trigeminal nerve and manifests as pain and a blister rash along the path of the nerve.
- Atypical Odontalgia presents as tooth pain with no obvious dental cause.
- Central Sensatisation is sensatisation of the dorsal horn and central structures that causes secondary hyperalgesia in the uninjured tissue around the injured site.
3. Vestibular Dysfunction can cause secondary headache and jaw pain. “The vestibular system is a complex system that includes the balance component of the inner ear and central nervous system structures. It’s primary functions are to sense linear and angular accelerations of the head, coordinate head and eye movements, and assist with the maintenance of equilibrium.” Dysfunction of the vestibular system can cause dizziness, vertigo, nausea, anxiety, neck pain and can also cause ear and jaw pain. As these symptoms can be similar to the symptoms of TMD, the vestibular system must be considered as a possible alternate cause of jaw pain.
4. Parotid Blockage by stones can cause pain and swelling over the parotid gland. This condition needs to be accurately diagnosed in order to exclude parotid tumours. Parotid blockage can respond to effleurage type massage and higher intensity ultrasound.
5. Benign or Malignant Tumours need to be excluded. They can cause ankylosis, contracture, loss of function and pain. These secondary problems may require treatment, once treatment of the tumour has been addressed.
6. Sinus Pain is caused by inflammation of the lining of the maxillary sinus. It is characterised by facial pain, headache, pain in the upper teeth, and a feeling of fullness on the affected side. Sinus pain may result in secondary cervical and TMJ pain.
7. Vascular pain or Headache
- Migraine with or without aura can be accompanied by nausea, vomiting, visual or auditory sensitivity. It can cause secondary tension or cervical headache. There is early evidence that indicates that treating neck dysfunction with physiotherapy can significantly reduce the severity and frequency of migraine. Dr Ian Devlin states “In the author’s experience the cervical spine has a very significant role in headache causation. Furthermore, some migraine sufferers report dramatic improvement in their migraine frequency and severity with competent management of their cervical spine dysfunction. In clinical practice, patients report that treatment of the cervical spine dysfunction by physiotherapists can reduce the frequency of migraine episodes.” At our practice we have found that treating neck stiffness, spasm and pain has reduced not only neck-related headache, but has also been helpful to our patients in reducing their migraine headache.
- Cluster Headaches are usually one sided and come in bouts lasting 30-60 minutes, with 1-3 attacks a day. It is more common in men and the pain is often excruciating. This type of headache doesn’t usually respond to physio, but treatment may help any secondary cervical or TMJ symptoms.
- Arterio-Venous Malformations such as temporal arteritis, can cause a moderate to severe headache in the temporal region. The pain is usually one sided and can refer to the face and neck. It is more common in older people, especially women and can be related to polymyalgia rheumatica. These patients need quick referral to a specialist as vision can be lost.
TMJ Disc Displacements
Introduction
Temperomandibular joint displacement, also known as internal disc derangement, is an abnormal relationship between the articular disc, the mandibular condyle and the mandibular fossa. The most frequent displacement of the disc is anterior to the mandibular condyle however, in rare cases it can be posteriorly. The prognosis for these conditions is good and normally recover with minimal intervention or conservative management.

Limited TMJ opening
Imaging studies have demonstrated that a more anterior disc position is relatively common in the asymptomatic population. It is also thought that in the majority of people the TMJ adapts to the disc position and rarely produces pain from being in a different position.
Clinical Presentation
Symptoms
- Pain or discomfort associated with anyone or combination of: chewing, yawning, talking, bruxism
- Headaches
- Ear pain
- TMJ range of movement may be restricted
- Crepitus/clicking during movement of the jaw
- Pain or discomfort can be acute or chronic that can fluctuate in intensity.
- Emotional issues such as depression is commonly associated with TMJ pain
Duration of symptoms may vary from hours to days.
Red flags
- Neurological signs
- Swelling
- Nose bleeding
- Dysphagia or dysarthria
- Unexplained weight loss
- Auditory complaints
- Constant pain unrelated to jaw movement
Types of TMJ disc displacement
- Disc displacement with reduction (DDWR): The articular disc displaces anteriorly to the condylar head, when the mouth is opened the disc relocates on the the condylar head.
- Hearing and palpating joint noises during opening and closing
- Protrusive opening and closings stops the reciprocal click
- There is unlikely to be any restriction in ROM due to the disc relocating when the mouth opens
- Disc displacement with reduction with intermittent locking: identical to DDWR with the additional symptom of intermittent limited jaw opening. This occurs when the disc does not reduce.
- Disc displacement without reduction (DDwoR) with limited opening: the articular disc displaces but does not reduce.
- TMJ pain
- Limited jaw range of movement <40mm
- Clicking and popping
- Disc displacement without reduction without limited opening: identical to DDwoR without limited ROM, although limited ROM must have occurred at some point.
These stages are under review and a new classification system is being trialled however at present it has only been trialled in adolescents. This classification reports five stages of disc displacement based on MRI results.
Diagnostic Procedures
Assessment of disc displacement can be done via subjective assessment, objective assessment and radiography.
Subjective assessment
The patient may have the history of:
- Insidious or traumatic onset
- Difficulty chewing food
- Reduced mouth opening
- Subjective clicking and popping
Objective Assessment
- Pain on TMJ palpation
- Potential clicking on jaw opening
- Reduced TMJ range of movement
- Associated muscular tightness of cervical and facial muscles such as sternocleidomastoid, upper trapezius and masseter.
Radiography
- XR
- Ultrasound can be useful in assessing the extent of disc derangement
- MRI is considered gold standard
Management/Intervention
Disc displacement without reduction
The best treatment plan for disc displacement without reduction is still under discussion and requires more evidence as treatment is usually based on experience rather than evidence.
Interventions can range from conservative management to surgical intervention. Although primary management for disc displacement should always be conservative.
Conservative management (primarily physiotherapy)
- Education and self-management
- Splinting
- Therapeutic exercise
- Joint mobilisation of the TMJ and cervical spine
- Active jaw exercises and strengthening
- Cognitive behavioural therapy
- NSAIDs and analgesia
Surgical intervention
- Arthrocentesis
- Arthroscopy
- Open joint intervenetion
On analysis of the surgical interventions there was no change in outcomes (pain and TMJ range of movement) when compared with each other.
Clinical bottom line
Regardless of intervention disc displacement without reduction has shown to improve over time, therefore the optimum treatment would be the least invasive and most cost effective i.e. education, self-management and early TMJ manipulation. In some extreme cases surgical intervention may be required but should be treated as a last choice.